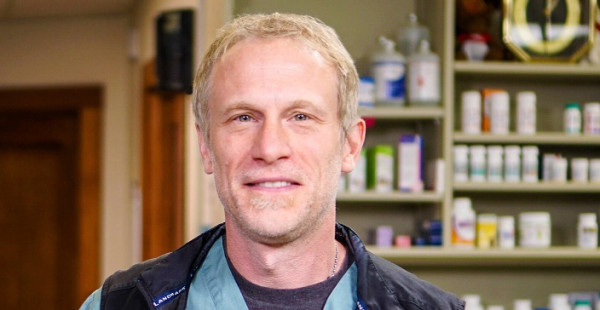
Søren Boysen, DVM, DACVECC is a Professor at the Department of Veterinary Clinical and Diagnostic Sciences, Faculty of Veterinary Medicine, University of Calgary. Søren is delivering four sessions at the Vets Now Emergency and Critical Care Congress, which is back in person after two years of virtual events.
The Congress will take place at The Royal Armoury in Leeds on November 3 and 4, with up to 80 hours of CPD.
What’s your veterinary background?
I graduated from the Western College of Veterinary Medicine in 1996 and spent a year in private practice on the west coast of Canada before completing a small animal internship at the Atlantic Veterinary College. I then spent a year at an emergency referral clinic in Chicago before starting a residency at Tufts University in Massachusetts. Following my residency, I returned to Canada as the Chief of Veterinary Emergency and Critical Care at the University of Montreal. I helped develop their ECC curriculum and created a post-graduate veterinary ECC residency training programme. After five years in Montreal, I moved to the University of Calgary Faculty of Veterinary Medicine, which has the newest vet school in Canada in 2009.
And what’s the appeal of ECC?
It’s the excitement of not knowing what’s coming through the door and then having only minutes or even seconds to figure out how to keep a patient alive. I wanted more than the routine I was seeing in private practice.
Tell us about your passion for ultrasound.
It was while at Tufts that my two mentors John Rush and Liz Rozanski encouraged me to do research. And, along with the radiology department and my resident mates, helped me establish the original FAST study in small animals. That would later evolve and become known as Point-of-Care Ultrasound. I love POCUS and I feel the applications are almost endless. Although, when I was in general practice initially, I struggled with ultrasound. I lacked confidence and when I started my residency only radiologists and cardiologists were permitted to use ultrasound. John said I’d be unlikely to get to use it unless I started a research project.
So, really believing there was an application for it and having a mentor who challenged me was what opened the door. I had no idea how big it would become, but POCUS is now pretty much the standard of care for the assessment of many emergency and critical care patients. I remember how frustrating ultrasound was for me prior to my residency, so we’ve tried to make it so that just about anyone can pick up an ultrasound probe and clinically apply it with confidence.
So, you have four sessions at Congress, the first being CPR POCUS – Using Ultrasound in Crashes, November 3 11.15.
This is quite a novel area in the human field of ECC, the application of ultrasound during cardiopulmonary arrest. When you have an arrest, they are using ultrasound in two ways to help find out what may be happening. They’re looking for underlying causes that may be reversible.
Most of us have had a patient who has arrested, and we’re trying to do CPR and resuscitate but we’re not going to succeed unless we know if there is an underlying cause that can be reversed. POCUS can help us find the specific problems that will help us manage the case differently.
The other application we’ve started to play with at the University of Calgary, and a couple of other groups in the US are researching, is using POCUS during active compressions. So, if you are doing a two-minute compression and you go to switch compressors as you should, I have a five-second window to look at that patient and assess the heart’s activity. It’s a real cutting-edge area of POCUS and we’re barely scratching the surface.
My hope is that people would be able to feel confident putting a probe on a patient, without disrupting compressions, to get a feel for what may be going on.
The first time I disagreed with a colleague November 3 12.45
It’s a reality of veterinary medicine that everyone has a strong opinion on one point or another and there are times we’ll disagree. So, I’m going to share some of the experiences in my earlier career where I disagreed, as well as similar instances later on. I’ll go through how we tried to resolve our differences. In a pressured environment, things can go sideways very quickly if there’s a strong disagreement, whether you’re a novice or a specialist. The biggest thing is how you handle that situation and take something positive from it for the future, even if we may not agree.
POCUS – the belly November 3 14.15
We’re going to look at abdominal POCUS, or APOCUS. We’ll be going through the 15 or so binary-driven questions we can answer with ultrasound. We’ll look at the basics, the original studies we started back at Tufts in 1999, the search for free fluid. Then we’ll evolve to look at the five common APOCUS sites, answering clinically relevant questions at each site. The aim is to provide evidence that non-specialists can quickly apply and answer POCUS questions in under five minutes which will help direct their management of patients.
Then POCUS – practical: November 3 16.30 with Lara Brunori is your final session.
This will be on ultrasound-guided vascular access and techniques wetlab. We will create phantoms that have imitation vessels and use ultrasound to help us walk catheters into them. You hit situations where placing a peripheral IV catheter is very difficult, perhaps because the patient is obese, has edema and you can’t feel that vessel. After I go through a demonstration of how I like to use ultrasound in those situations, those attending will work in small groups with an ultrasound machine and a phantom to practice. We’ll give them the hints and tips they need to hopefully get that catheter into the vessel or draw a blood sample. So, it will be very much hands-on.
And finally, what are you most looking forward to about having the Congress in-person this year?
I really enjoy the Vets Now Congress as there’s such a great group of people who are very ECC-focused. As well as catching up with colleagues, I love the social component. There’s such a great balance between the two. I’ve attended at Harrogate twice and there’s usually a nice dress-up social event – so I’m going to have to figure out the theme and make sure I have a costume this year!